Fungi have always been in the background, but things changed with a recent discovery in China. A novel fungal pathogen, Rhodosporidiobolus fluvialis, has become a topic of concern for global health authorities. As if this drug-resistant fungus is in need of any more concern, it also has the ability to evade common antifungal drugs and has the disturbing capacity to evolve rapidly in warmer conditions. With climate change looming over everything, R. fluvialis might serve as an early indicator of an upcoming health crisis.
What is Rhodosporidiobolus fluvialis?
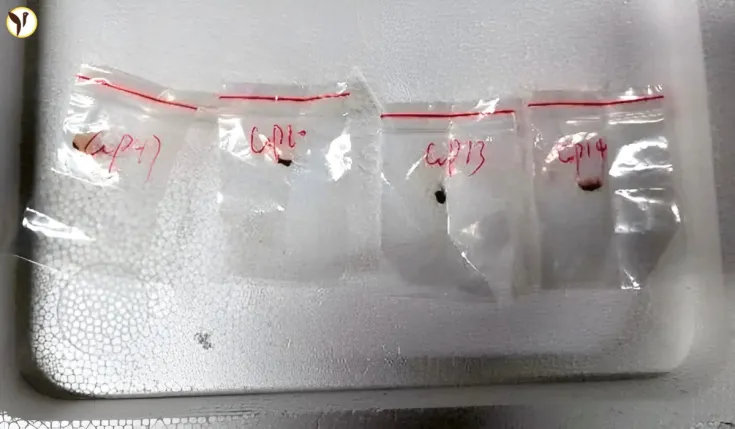
Recently, sandwiching clinical samples from two different patients from separate Chinese regions revealed novel Rhodesoporidiobolus fluvialis. Both infected patients had existing comorbidities that made them more susceptible to infection. While the discovery of a new fungal species may not sound troubling at face value, the distinguishing features of R. fluvialis are rather alarming:
- Drug Resistance: Laboratory evaluations have disclosed that R. fluvialis seems to be impervious to some of the more common drugs employed in treating fungal infections like fluconazole and caspofungin.
- Mutation Capacity: The fungus was capable of rapid evolution, due to undergoing a high mutation rate at a human body temperature. These sorts of mutations can make the pathogen harder to treat and more virulent.
Adaptability of the fungus is causing more alarm to scientists, as it suggests that the pathogen has potential to become more harmful over time.
Rhodosporidiobolus fluvialis :: New fungal infection discovered in China https://t.co/fJc3IvN86o
— Wally Pons (@wallypons) July 18, 2024
What is Currently Increasing the Incidence of Fungal Disorders
While bacteria and viruses have always dominated the scene of diseases, fungi have remained sparsely focused on. The emerging issues regarding the fungal pathogens posing risks to public health is heightened by the discovery of R. fluvialis. One of the key contributors to this rise is the change in global climate.
This is how increasing global temperatures can be connected to the issue:
- Human Host Adaptation: The majority of fungi are more confortable in cool, outdoor environments, and infecting humans rarely happens, as the human body is too hot to be one. Some fungi, however, are evolving to survive at higher temperatures, which makes them more likely to infect humans as climate change intensifies.
- Mutation Rationale: Accelerated change in temperature acts like a R. fluvialis incubator. Increased temperature leads to accelerated fungal mutation, enhancing the chances of emerging strains becoming infectious and more resistant to drugs.
- Global Dissemination: Shifts in climate, tourism, and commerce allow fungi greater access to new regions and populations.
The finding of R. fluvialis serves as a striking example of what climate change may create in the future—it may increase the likelihood of fungi infections switching from environmental ailments (using the term ‘pathogen’) to threats to human health.
Current Status of the Fungus
The positive aspect is that there is no need to panic just yet. There are only two documented cases of R. fluvialis infections, and there is no sign for uncontrolled transmission as of now. Both cases were reported in patients who are immunocompromised.
However, experts say not to relax too much. Especially in vulnerable healthcare settings, fungal infections can lie dormant and go unnoticed before suddenly becoming widespread. Previous outbreaks of the drug-resistant fungus, Candida auris, have demonstrated how healthcare systems were caught off guard. If no action is taken, however, R. fluvialis could follow the same path.
The Growing Concern Around Antifungal Resistance
Antifungal resistance is brewing as a formidable obstacle to modern medicine. There are many antibiotics available for bacterial infections, whereas antifungal drugs are more limited in number, and increasing reports of antifungal resistant pathogens, such as R. fluvialis, reveal the failing antifungal arsenal.
There are several reasons antifungal resistance is a growing concern, including:
- Overuse of antifungals: Although antifungal resistance may be similar to antibiotic resistance from overuse, antifungals are often seen as less of a risk, leading to overuse of antifungals in both agricultural and healthcare settings. Excessive use of antifungals in agriculture are contributing significantly to the growing problem of antifungal resistance.
- Underinvestment: Historically, there has been less funding for fungal research and development of therapeutic agents compared to bacterial and viral disease research. Consequently, we as health providers lack available options to deal with emerging threats.
- Delayed diagnosis: Overall, fungal infections are notoriously challenging for early diagnosis, and so any delay leads to greater proliferation and opportunity for pathogens to develop resistance.
If pathogens like R. fluvialis sway resistance from the few available antifungal agents, the consequences could be catastrophic, especially for patients with impaired immune systems.
How to keep yourself protected:
R. fluvialis poses no threat in the present time, however, it is important to stay on guard. The following mentioned steps will help you lower the chances of contracting fungal infections:
Follow Good hygiene:
- Wash your hands after public and hospital visits.
- Disinfect surfaces that are frequently touched like door handles and countertops.
Preventative measures:
- For the immunocompromised out there, consult with your physician for precautionary measures.
- Avoid dusty regions in hospitals since these areas tend to harbor and spread pathogens through dust particles.
Keep Unusual Symptoms in Mind
- Fever, fatigue without reason, or breathing issues could indicate a dangerous fungal infection. It's critical that you see a doctor right away to address unresolving symptoms.
Follow Reliable Updates
- Keep abreast of changes or updates to public health policies, particularly outbreaks of fungal diseases.
Fungi’s Real Threat
Mushrooms on your pizza and moldy bread might not strike the average person as posing any threat, however fungi have become stealthy contenders for the most dangerous global health concern. This is why:
- Lack of Attention: Fungal diseases are overlooked compared to viral or bacterial infections. This produces lower public attention and, subsequently, funding.
- More Difficult to Treat: Whereas antibiotics may easily treat a bacterial infection, antifungal treatments are far more scarce. Certain fungal infections may require lengthier and costlier treatment plans.
- Strain Issue: Climate change, global traveling, and increasing rates of immunocompromised conditions (diabetes, cancer, organ transplants) tend to create conditions that foster fungal infections.
Increased terrority for public health focuses on surveillance and prompt diagnostic testing, as well as supplementary funding towards antifungal drug research.
How to Take Action and Stay Informed
The development of Rhodosporidiobolus fluvialis indicates the need to incorporate fungal pathogens in the health discourse, which, until now, has been ignored. Combined with rising temperatures and increasing cases of polydrug resistance, it becomes crucial to act immediately.
On a personal level, awareness and self-care is the foremost priority. On a systemic level, it is mandatory to funnel resources towards fungal studies and proactive surveillance.
Preparedness will ensure information, which helps mitigate potential crises, will remain under control.
Image Source: The Guardian